Patient Safety Indicators
At Mackenzie Health, quality care and patient safety are our top priorities.
We believe in being accountable and transparent with the community about our performance and providing quality services. The Infection Prevention and Control (IPAC) Department is devoted to protecting patients from hospital acquired infections. Hospital infection rates are regularly monitored and used to continually improve patient care and safety.
Sometimes when patients are admitted to the hospital, they can contract infections. These are called hospital-acquired or nosocomial infections. Hospital-acquired mean that the infection is identified 72 hours after admission to the hospital; or that the infection was present at the time of admission but was related to a previous admission to that hospital within the last four weeks.
At Mackenzie Health, the following practices are in place to help prevent transmission of organisms within the hospital setting:
- Follow provincial and federal best practice guidelines
- A collaborative antibiotic stewardship program to provide education and review antimicrobial use in the hospital
- Aggressive environmental cleaning processes and routine environmental audits
- Robust education and hand hygiene program
- Comprehensive surveillance, disease investigation and outbreak management
Patient Indicators and Reporting
The Ontario Ministry of Health and Long-Term Care has established several patient safety indicators that all hospitals are required to publicly report. We suggest that you to review our results through the tabs below. For more information on patient safety reporting, please visit here.
Clostridiodes difficile (also known as C.diff) is a type of bacteria found in the intestinal tract. It causes inflammation in the colon which may cause symptoms of diarrhea, fever and stomach pain.
The use of antibiotics increases the chances of developing C.diff. Both the development of C.diff and the number of patients receiving antibiotics can lead to outbreaks of C. diff in hospitals.
The following data represents monthly hospital acquired Clostridiodes difficile cases per 1,000 patient days at Mackenzie Health. The total patient days represents the sum of the number of days during which services were provided to all inpatients, over one year of age, during the given time period.
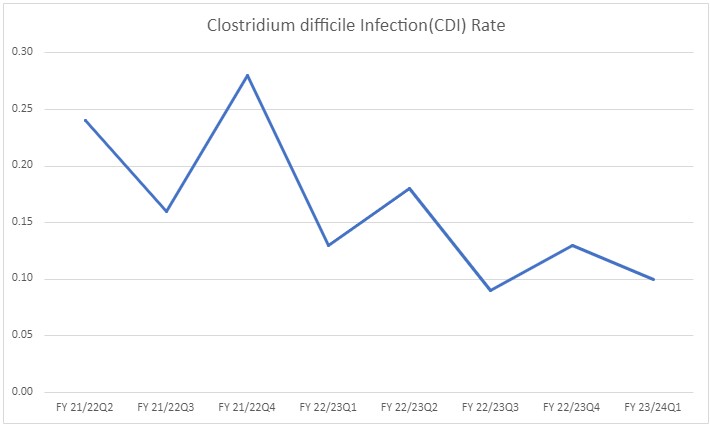
| Quarter End Date | Fiscal Period | Clostridium difficile Infection (CDI) Rate |
| 6/30/2023 | FY 23/24Q1 | 0.10 |
| 3/31/2023 | FY 22/23Q4 | 0.13 |
| 12/31/2022 | FY 22/23Q3 | 0.09 |
| 9/30/2022 | FY 22/23Q2 | 0.18 |
| 6/30/2022 | FY 22/23Q1 | 0.13 |
| 3/31/2022 | FY 21/22Q4 | 0.28 |
| 12/31/2021 | FY 21/22Q3 | 0.16 |
| 9/30/2021 | FY 21/22Q2 | 0.24 |
| 6/30/2021 | FY 21/22Q1 | 0.16 |
| 3/31/2021 | FY 20/21Q4 | 0.21 |
| 12/31/2020 | FY 20/21Q3 | 0.08 |
| 9/30/2020 | FY 20/21Q2 | 0.19 |
A central venous catheter (or "line") is put into a patient's vein, usually when they require long-term access to medication, fluids, or nutrition intravenously (through an IV). A central line infection can occur when bacteria and/or fungi enter the bloodstream, causing a patient to become sick.
The following data represents the monthly Intensive Care Unit (ICU) Central Line Infection (CLI) cases at Mackenzie Health in the past per 1000 central line days. The CLI rate is the number of ICU patients (18 years and older) with a new CLI per 1,000 central line days. Central line days are the total number of days a central line was used in ICU patients who are 18 years and older.
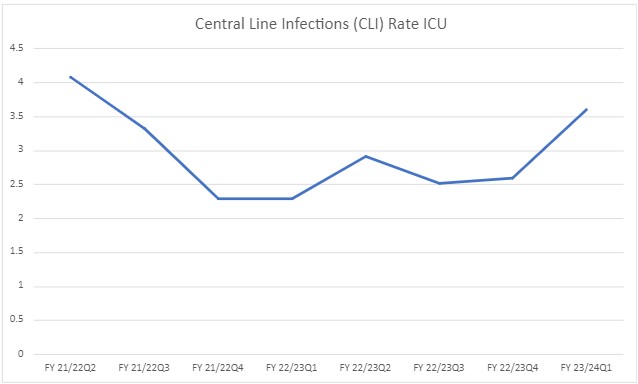
| Quarter End Date | Fiscal Period | Central Line Infections (CLI) Rate ICU |
| 6/30/2023 | FY 23/24Q1 | 3.6 |
| 3/31/2023 | FY 22/23Q4 | 2.6 |
| 12/31/2022 | FY 22/23Q3 | 2.52 |
| 9/30/2022 | FY 22/23Q2 | 2.92 |
| 6/30/2022 | FY 22/23Q1 | 2.31 |
| 3/31/2022 | FY 21/22Q4 | 2.29 |
| 12/31/2021 | FY 21/22Q3 | 3.33 |
| 9/30/2021 | FY 21/22Q2 | 4.08 |
| 6/30/2021 | FY 21/22Q1 | 5.61 |
| 3/31/2021 | FY 20/21Q4 | 4.47 |
| 12/31/2020 | FY 20/21Q3 | 6.66 |
| 9/30/2020 | FY 20/21Q2 | 4.77 |
The most common mode of transmission of health care-associated infections (HAIs) in healthcare settings is via the hands of health care workers that have touched colonized or infected patients or contaminated material or equipment. Hand hygiene is the single most effective way to reduce the risk of healthcare-associated infections. Through auditing the practices of our health care providers, we can determine if they are cleaning their hands – the right way, at the right times and following the Ontario Ministry of Health's guidelines. Using hand sanitizer is the preferred way to clean one’s hands, except when hands are visibly soiled, then washing hands with soap and water is the best method.
Hand Hygiene Compliance Rate
Hospitals across Ontario are required to audit and report their hand hygiene compliance rates annually based on two indicators: before the initial patient or patient environment contact and after the patient or patient environment contact.
The following data represents hand hygiene compliance collected through direct observation amongst Mackenzie Health staff in the past two years.
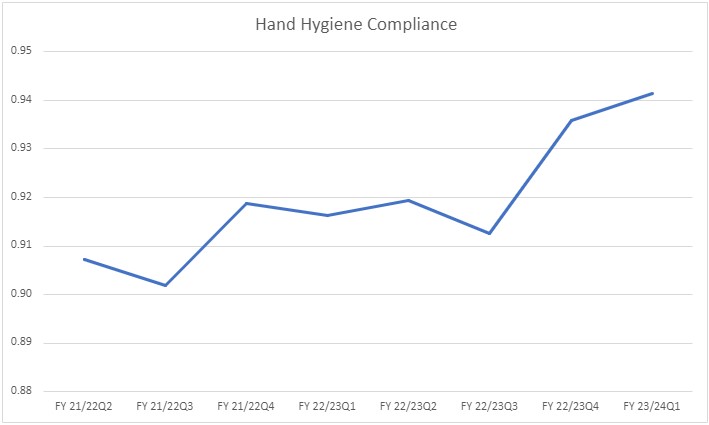
| Quarter End Date | Fiscal Period | Hand Hygiene Compliance |
| 6/30/2023 | FY 23/24Q1 | 0.94 |
| 3/31/2023 | FY 22/23Q4 | 0.94 |
| 12/31/2022 | FY 22/23Q3 | 0.91 |
| 9/30/2022 | FY 22/23Q2 | 0.92 |
| 6/30/2022 | FY 22/23Q1 | 0.92 |
| 3/31/2022 | FY 21/22Q4 | 0.92 |
| 12/31/2021 | FY 21/22Q3 | 0.90 |
| 9/30/2021 | FY 21/22Q2 | 0.91 |
| 6/30/2021 | FY 21/22Q1 | 0.84 |
| 3/31/2021 | FY 20/21Q4 | 0.75 |
The Ministry of Health requires that all hospitals publicly report their Hospital Standardized Mortality Ratio (HSMR).
What is HSMR and what does it measure?
HSMR stands for hospital standardized mortality ratio. It is the ratio of observed death over expected death for the top 80% of admission diagnoses, comparing an individual hospital's mortality rate with the average Canadian rate. A ratio of 100 means that the hospital mortality rate is equal to the national average. At Mackenzie Health, we continuously aim to have mortality rates lower than the national average.
Why is HSMR important?
HSMR is a broad quality indicator and a measure that help hospitals follow trends in their hospital mortality rates. Trends in HSMR can be used by hospitals to moniter and improve quality of care and patient safety.
What is Mackenzie Health doing to Improve Quality of Care and Patient Safety?
Mackenzie Health tracks HSMR regularly and reports it throughout the organization . Quality improvement projects and processes such as Zero Harm, Quality Aims, High Reliability, and Morbidity & Mortality Conferences help improve quality of care and patient safety.
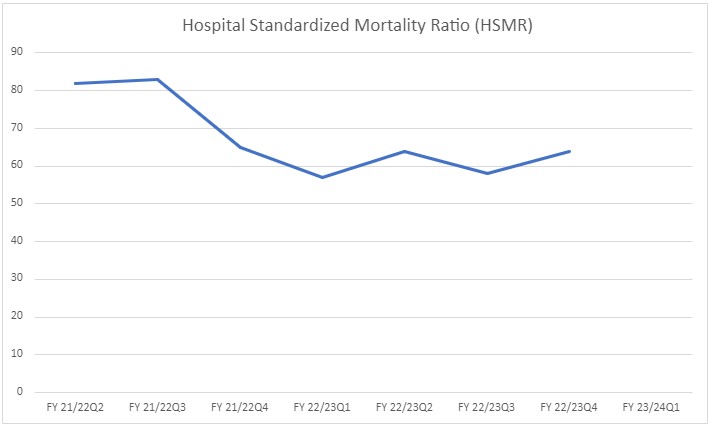
| Quarter End Date | Fiscal Period | Hospital Standardized Mortality Ratio (HSMR) |
| 6/30/2023 | FY 23/24Q1 | #N/A |
| 3/31/2023 | FY 22/23Q4 | 64 |
| 12/31/2022 | FY 22/23Q3 | 58 |
| 9/30/2022 | FY 22/23Q2 | 64 |
| 6/30/2022 | FY 22/23Q1 | 57 |
| 3/31/2022 | FY 21/22Q4 | 65 |
| 12/31/2021 | FY 21/22Q3 | 83 |
| 9/30/2021 | FY 21/22Q2 | 82 |
| 6/30/2021 | FY 21/22Q1 | 61 |
| 3/31/2021 | FY 20/21Q4 | 94 |
| 12/31/2020 | FY 20/21Q3 | 83 |
| 9/30/2020 | FY 20/21Q2 | 76 |
Methicillin-Resistant Staphylococcus aureus (MRSA) is a type of Staphylococcus aureus normally found on the skin and in the nose of many healthy people. This is called carriage or colonization. Methicillin is an antibiotic developed specifically to treat infections caused by Staph aureus.
MRSA is a type of Staphylococcus aureus that is resistant to most antibiotics, including the antibiotic methicillin. MRSA can cause many types of infection, including wound and surgical site infections, bloodstream infections (bacteremia) and pneumonia.
The following data represents the rate of new hospital-acquired MRSA bacteremia per 1,000 patient days at Mackenzie Health in the past two years. The total patient days represents the sum of the number of days during which services were provided to all inpatients, over one year of age, during the given time period.
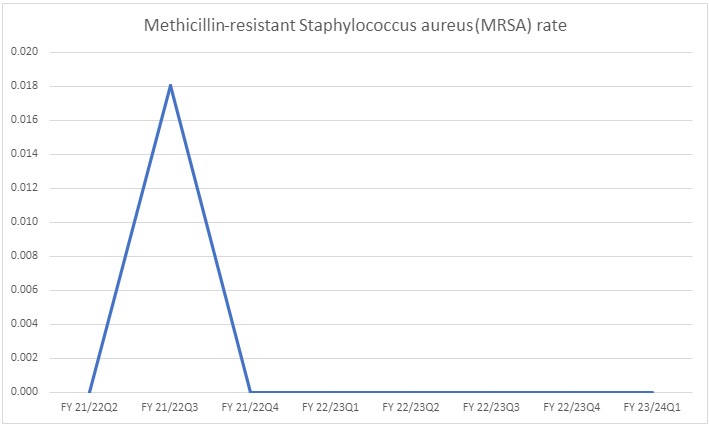
| Quarter End Date | Fiscal Period | Methicillin-resistant Staphylococcus aureus (MRSA) rate |
| 6/30/2023 | FY 23/24Q1 | 0.000 |
| 3/31/2023 | FY 22/23Q4 | 0.000 |
| 12/31/2022 | FY 22/23Q3 | 0.000 |
| 9/30/2022 | FY 22/23Q2 | 0.000 |
| 6/30/2022 | FY 22/23Q1 | 0.000 |
| 3/31/2022 | FY 21/22Q4 | 0.000 |
| 12/31/2021 | FY 21/22Q3 | 0.018 |
| 9/30/2021 | FY 21/22Q2 | 0.000 |
| 6/30/2021 | FY 21/22Q1 | 0.000 |
| 3/31/2021 | FY 20/21Q4 | 0.000 |
| 12/31/2020 | FY 20/21Q3 | 0.000 |
| 9/30/2020 | FY 20/21Q2 | 0.000 |
Enterococci are common bacteria that are normally found in the bowel, and the female genital tract and are often found in the environment. Vancomycin is a powerful antibiotic used to treat serious infections. Vancomycin-resistant enterococci (VRE) are a type of bacteria that no longer responds to treatment with vancomycin.
Healthy people are usually not at risk of becoming infected with VRE. Risk factors for getting VRE include the severity of underlying illness, presence of invasive devices, prior colonization with VRE, antibiotic use, and length of hospital stay. VRE can cause illnesses such as blood infections (bacteremia), urinary tract infections, or abscesses.
The following data represents the new hospital-acquired VRE Bacteremia cases at Mackenzie Health in the past two years. The total patient days represents the sum of the number of days during which services were provided to all inpatients, over one year of age, during the given time period.
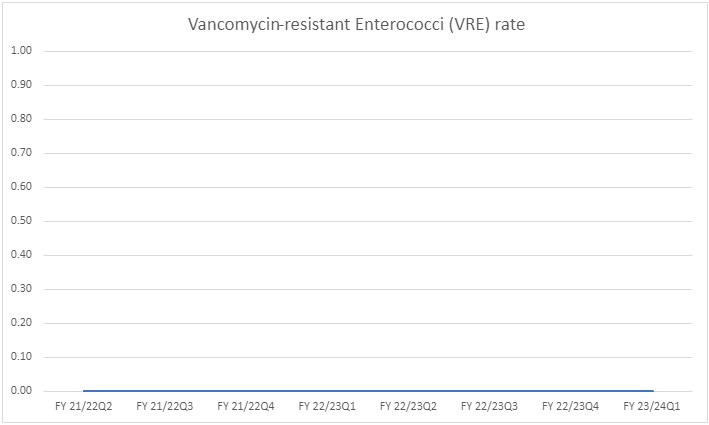
| Quarter End Date | Fiscal Period | Vancomycin-resistant Enterococci (VRE) rate |
| 6/30/2023 | FY 23/24Q1 | 0.000 |
| 3/31/2023 | FY 22/23Q4 | 0.000 |
| 12/31/2022 | FY 22/23Q3 | 0.000 |
| 9/30/2022 | FY 22/23Q2 | 0.000 |
| 6/30/2022 | FY 22/23Q1 | 0.000 |
| 3/31/2022 | FY 21/22Q4 | 0.000 |
| 12/31/2021 | FY 21/22Q3 | 0.000 |
| 9/30/2021 | FY 21/22Q2 | 0.000 |
| 6/30/2021 | FY 21/22Q1 | 0.022 |
| 3/31/2021 | FY 20/21Q4 | 0.000 |
| 12/31/2020 | FY 20/21Q3 | 0.000 |
| 9/30/2020 | FY 20/21Q2 | 0.000 |
Surgical Site Infection (SSI) is an infection that occurs after a surgery, in the part of the body where the surgery took place. Mackenzie Health is a participant in the National Surgical Quality Improvement Program (NSQIP), that allows Mackenzie Health to compare infection rates to hundreds of hospitals internationally and apply best practices from these hospitals within Mackenzie Health for the prevention of SSI. Best practice for administration of pre-operative antibiotics ensures that antibiotics are administered within the currently recommended 60-minute time frame (120-minutes for Vancomycin).
The departments of surgery and anesthesia, the peri-operative service, and infection control to work together to create programmatic change that will ensure that all our patients receive the best care possible.
The following table represents the antibiotic timing rate at Mackenzie Health before a hip or knee replacement surgery for patients 18 years and older.
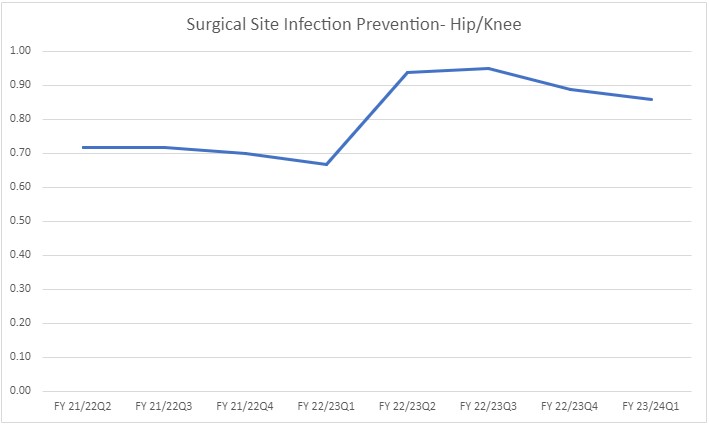
| Quarter End Date | Fiscal Period | Surgical Site Infection Prevention - Hip/Knee |
| 6/30/2023 | FY 23/24Q1 | 0.86 |
| 3/31/2023 | FY 22/23Q4 | 0.89 |
| 12/31/2022 | FY 22/23Q3 | 0.95 |
| 9/30/2022 | FY 22/23Q2 | 0.94 |
| 6/30/2022 | FY 22/23Q1 | 0.67 |
| 3/31/2022 | FY 21/22Q4 | 0.7 |
| 12/31/2021 | FY 21/22Q3 | 0.72 |
| 9/30/2021 | FY 21/22Q2 | 0.72 |
| 6/30/2021 | FY 21/22Q1 | 0.67 |
| 3/31/2021 | FY 20/21Q4 | 0.94 |
| 12/31/2020 | FY 20/21Q3 | 0.8 |
| 9/30/2020 | FY 20/21Q2 | 0.71 |