Professional Practice and Education
The Professional Practice and Education Team champions evidence-based best practices across Mackenzie Health for all Regulated Health Care Professionals through the use of a framework called a Professional Practice Model.
What is a Professional Practice Model?
A Professional Practice Model is the driving force of clinical care.
Mackenzie Health’s Professional Practice Model was developed by our frontline staff through an appreciative inquiry process in 2020. Over 500 clinicians (31% of our clinical workforce) were directly engaged as active participants in the development of this model, with the final model representing our collective values and priorities as a collaborative care team.
Shared values shape our behaviour and lead the way for continuous quality improvement driven by frontline initiatives.
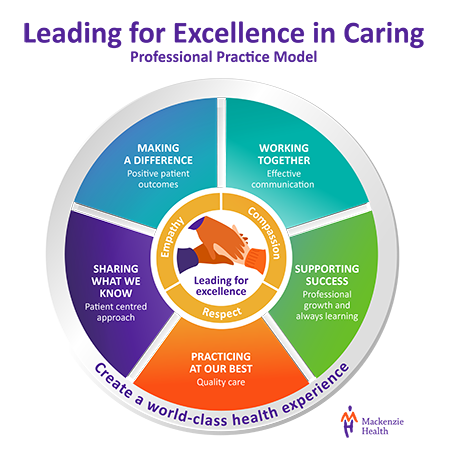
Our model depicts how we as clinicians are:
- Working Together using collaborative care approaches to deliver excellent quality care to every patient, every time
- Supporting Success of our peers, our teams, and our patients
- Practicing at our Best by using effective and efficient processes to measure, evaluate, and relentlessly improve care
- Sharing What We Know with our patients and each other, to ensure that we are consistently learning through active listening and seeking out new knowledge
- Making a Difference by valuing what matters to you, our patients. We care for you as we would expect our own family to be cared for, and with our person-centred care values of Compassion, Empathy, and Respect.
Everything that we do to improve care outcomes and guide our principles for Professional Practice, Care Delivery and Education.
Meet the Collaborative Care Team at Mackenzie Health
Registered Nurse (RN) or Registered Practice Nurse (RPN):
- Most patients will interact with a nurse during their visit to Mackenzie Health.
- Nurses provide care for people of all ages, families, groups, and communities and in all settings
- Nurses promote health, prevention of illness, and the care of well, ill, disabled and dying people
- Nurses have a role in patient advocacy, education, promoting safety, research, shaping health policy and health systems management
- Occupational therapists work with the barriers that may affect a patient’s participation in daily activities by teaching new ways of doing things using materials or equipment that makes life easier or adapting their environment to work better for them.
- Maximizing participation in activities of daily of living (ADL’s) that have personal meaning and value by assisting with restoring physical and cognitive function.
- Play a key role in discharge planning. This may include providing suggestions for services upon discharge home, referral to rehab programs or providing equipment recommendations.
- Physiotherapists provide in depth assessment and analysis of patients presenting with a variety of acute and chronic conditions that affect their ability to manage and navigate their daily lives.
- Physiotherapists play an integral role in discharge planning from a hospital setting and collaborate extensively with other members of the inter-professional team.
- Physiotherapists at Mackenzie Health can be found across the entire hospital in the areas of ED, Critical Care Unit, acute medicine, acute surgery, orthopedic rehab, stroke (ISU), complex continuing care, slow stream rehab, and day surgery. We also provide on-call care to other areas such as Pediatrics and Mental Health
Registered Respiratory Therapists
Registered Respiratory Therapists play an essential role in providing quality and patient/family centered care. Registered Respiratory Therapists are responsible for monitoring, assessing and providing treatment and education of cardio-respiratory and associated disorders.
Registered Respiratory Therapists are highly trained in:
- Ventilation and airway management
- Cardiopulmonary resuscitation (CPR)
- Oxygen and aerosol therapy
Registered Respiratory Therapists provide services to all areas of the hospital including:
- Critical Care Units
- Emergency Department
- Medical and Surgical Ward Units
- Complex Continuing Care
- Peri-Op
Certified Clinical Anesthesia Assistants are Registered Respiratory Therapists who have received advanced training in Anesthesia Assistant program. They participate in the care of the stable surgical patient during general, regional, or conscious sedation anesthesia through medical directives under the supervision of the anesthesiologist.
Registered Dietitians are integral members of the health care team at Mackenzie Health, ensuring patients meet their nutritional needs based on their illness or condition.
Mackenzie Health dietitians are the nutrition experts and help to:
- treat, counsel and support patients by promoting or maintaining health,
- improve nutritional status
- preventing malnutrition in hospitals and communities
- recommend medical nutrition therapy including oral diet modification and or supplementation, including invasive nutrition support techniques such as enteral nutrition or parenteral nutrition.
- Provide diet teaching, patient and family education and lifestyle changes for safe discharge
- identify and understand sources of stress or difficulty
- develop coping skills
- find effective solutions to problems
- provide resources
- assist in discharge planning and,
- provide emotional support and counselling to patients & their families.
Speech-language Pathologists (SLP) at Mackenzie Health identify, assess, and treat patients presenting with swallowing, speech, language, and cognitive-communication disorders.
They identify the functional status of a patient's swallow and provide intervention to maximize patient safety and quality of life. An SLP may conduct clinical swallowing evaluation at your bedside or using a videofluoroscopic swallowing assessment in the medical imaging department.
Medical Radiation Technologists
Medical Radiation Technologists work with almost all departments to provide diagnostic medical imaging services across the organization, both in the Medical Imaging department as well as in patient care areas.
Medical Laboratory Technologists
Help and assist physicians diagnose and treat patients, as well as monitor and prevent diseases through laboratory testing, diagnoses, and analysis.
Medical Laboratory Technologist may come to take a blood sample, or other specimen, after a doctor, midwife, dentist, or nurse practitioner orders a test for you.
Pharmacy Services encompasses two regulated healthcare professions – pharmacy technicians and pharmacists
- Pharmacy technicians are primarily responsible for technical aspects of medication distribution but are also present in ED to help collect Best Possible Medication History (BPMH). A BPMH is collected at the beginning of a patient’s journey in the hospital and is the starting point for ensuring that the patient will receive the right medications during and after their hospital visit.
- Pharmacists provide drug information to both patients and other healthcare providers. Pharmacists provide insulin pen and inhaler teaching, as well as group classes in Cardiac Rehab and Mental Health. We also perform discharge counselling if needed when patients are going home with new or changed medications.
- Pharmacists review drug interactions and monitor for effectiveness and side effects.
The Professional Practice and Education Team champions evidence-based best practices across Mackenzie Health for all Regulated Health Care Professionals through the use of a framework called a Professional Practice Model.
There are Professional Practice and Education Leaders for all interprofessional disciplines that support Standards of Practice focused on achieving excellence in practice.
Professional Standards of Practice
Are formal statements established by the various Regulatory Colleges in Ontario. These standards guide and inform health care professionals and consumers as to the expectations of patient/client care and are designed to ensure that professionals are effective in delivering patient/client care in a timely, safe, and effective manner.
Professional Practice and Education Leaders
A Professional Practice Leader or Educator supports clinicians in all patient care areas. These roles are representative voices of the profession and focus on education and clinical practice support, as well as shared decision making.
Interprofessional Orientation
At Mackenzie Health, we provide support to all of our interprofessional staff regardless of the level of your experience. We want you to make Mackenzie Health your "career" home.
We have developed an Interprofessional Orientation Program for newly hired professionals to support and assist them as they transition into their new roles. The goal of the Interprofessional Orientation Program is to promote clinical excellence, interprofessional collaboration and their role in improving the patient and family's experience of care at Mackenzie Health.
Topics covered during Interprofessional Orientation include, but not limited to:
- Professional Standards & Scopes of Practice
- Patient and Family Centered Care
- Collaborative Care Delivery
- Quality Improvement and Patient Safety
- Medical Ethics
- Seniors Friendly Care Strategies
- Least Restraint and Behavioural Care Planning
- Falls Prevention, Safe Mobilization and Transfers
- Infection Prevention and Control
Clinical Skills and Practice
Clinical Practice at Mackenzie health is driven by evidence and best practices, and is sustained through organizational policies and procedures.
These bursaries provide financial support for nurses and allied health care professionals to advance their practice through professional development.
To apply, please visit Bursary Awards - Mackenzie Health and select which bursary you would like to apply to.